Pain Does Not Always Equal Damage: Understanding Sensitive Nervous Systems
Pain is one of the most powerful signals the body has. When something hurts, it feels natural to assume that something must be damaged, injured, or worsening. While that can sometimes be true — especially with acute injuries — pain does not always reflect tissue damage.
In fact, many people experience persistent pain even after tissues have healed, imaging looks normal, or surgery was technically “successful.” Understanding why this happens can be one of the most important steps toward recovery.
Pain Is a Protection System — Not a Damage Meter
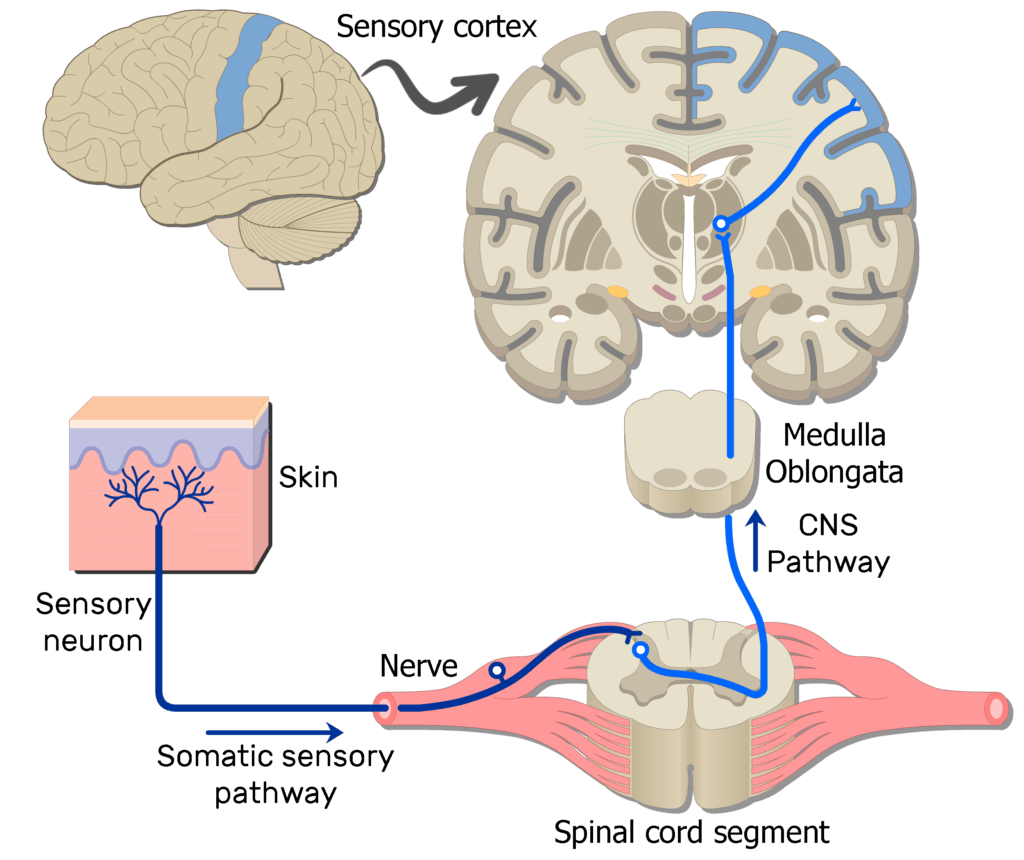
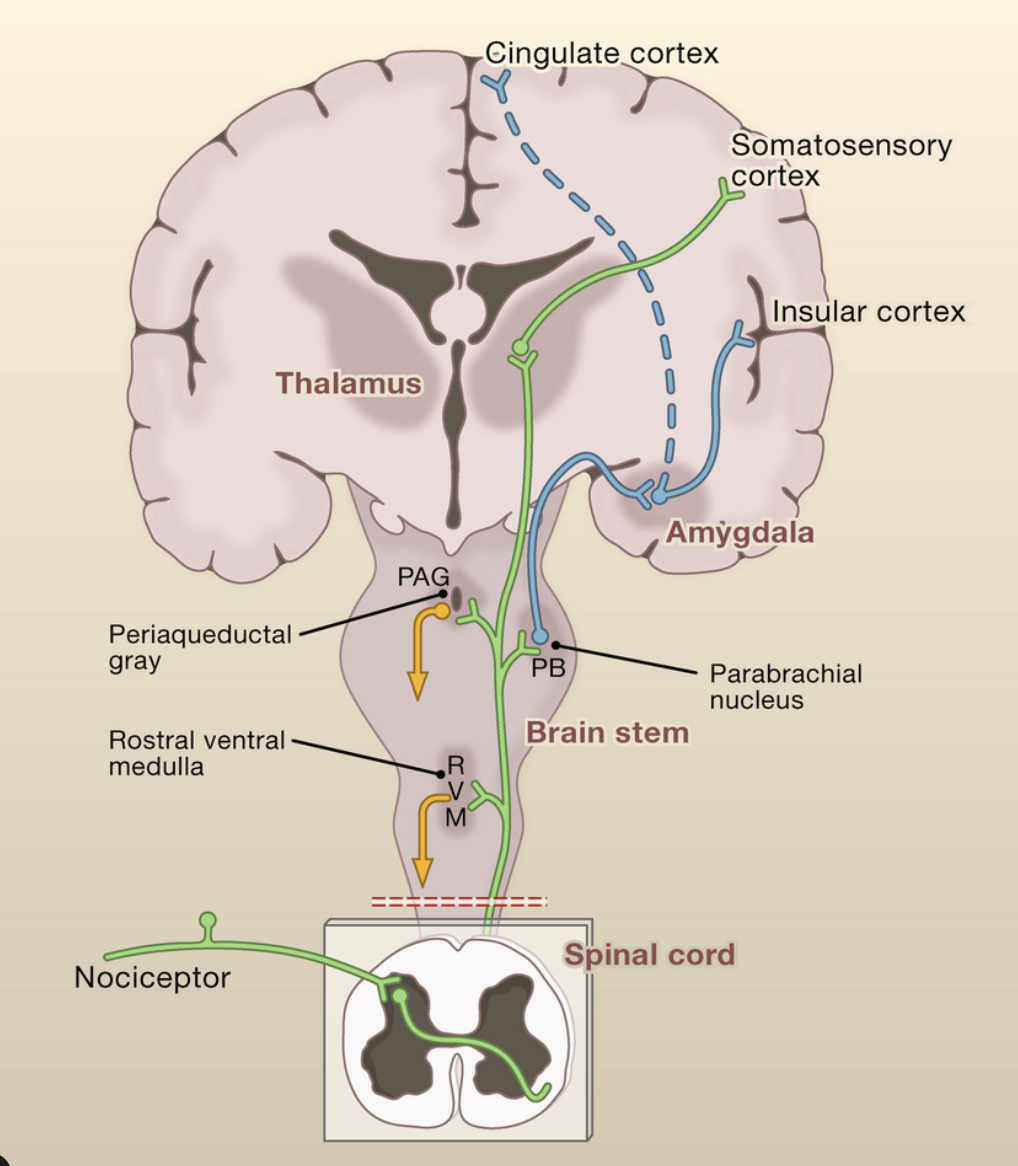
Pain is best understood as a protective response, not a direct measurement of injury. Its job is to warn the brain of potential threat and encourage us to change behavior.
Think of pain like a smoke alarm. A smoke alarm is meant to alert you to danger — but sometimes it goes off when you burn toast. The alarm is real, loud, and disruptive, but it doesn’t mean your house is on fire.
Similarly, pain can be very real and intense even when tissues are not being damaged.
When the Nervous System Becomes Overprotective
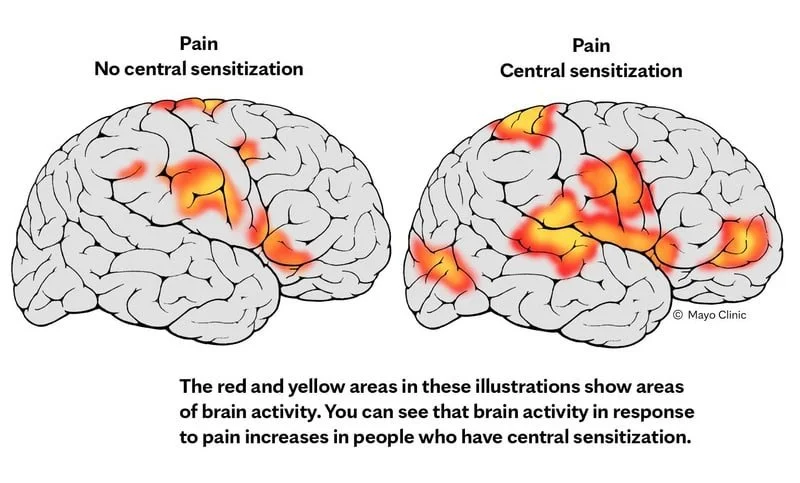
After an injury, surgery, or repeated flare-ups, the nervous system can become more sensitive. This means it starts reacting to lower levels of stimulus than it used to.
Instead of needing a strong signal to trigger pain, the system begins firing alarms more easily — during normal movements, light loads, or even positions that were once comfortable.
This heightened sensitivity can persist long after tissues have healed. It’s not because the body is broken — it’s because the nervous system has learned to be extra cautious.
This is often referred to as pain sensitivity or central sensitization, but the key takeaway is simple:
👉 Your system is trying to protect you — it’s just overdoing it.
Why Imaging Doesn’t Always Explain Pain
One of the most frustrating experiences for patients is being told:
“Your MRI looks normal”
“There’s nothing structurally wrong”
“We don’t see anything concerning”
Yet the pain is still there.
Imaging shows structure — not sensitivity. Many people without pain have disc bulges, arthritis, or tendon changes. At the same time, many people with pain show little or nothing abnormal on scans.
Pain is influenced by:
Previous injuries
Fear or guarding
Stress and fatigue
Sleep quality
Activity spikes or deconditioning
Nervous system sensitivity
These factors don’t show up on imaging — but they strongly affect how pain is experienced.
This Pain Is Real — Not “In Your Head”
Understanding pain sensitivity does not mean pain is imaginary, exaggerated, or psychological.
Pain is a real biological experience created by the nervous system. When the system becomes hypersensitive, the pain output increases — even if tissue damage is minimal or absent.
This is why people can feel:
Pain with light movement
Symptoms that fluctuate day to day
Discomfort that spreads or changes location
Pain that lingers longer than expected
Recognizing this actually validates the experience rather than dismissing it.
Why “Pushing Through It” Often Backfires
When pain is driven by sensitivity rather than damage, aggressive approaches often make things worse.
Trying to:
Force stretches
Push through sharp pain
Ignore symptoms completely
Rush strength or return to sport
can reinforce the nervous system’s belief that movement is dangerous.
Instead of calming things down, this teaches the system to stay on high alert.
How Pain Sensitivity Improves
The encouraging part is that nervous system sensitivity can be retrained.
The goal is not to avoid movement — it’s to reintroduce it in a way that feels safe, controlled, and progressive.
Effective rehab often focuses on:
Gradual exposure to movement
Finding tolerable starting points
Building confidence before intensity
Improving strength and endurance slowly
Educating patients on what sensations mean
As the nervous system learns that movement is safe again, pain signals often decrease — sometimes dramatically.
Why Education Matters in Recovery
Understanding why pain behaves the way it does can reduce fear, and reduced fear often leads to better movement.
When patients stop interpreting every symptom as damage, they:
Move more naturally
Guard less
Recover faster
Feel more in control
Education isn’t just reassurance — it’s a therapeutic tool.
What This Means for Physical Therapy
Physical therapy isn’t just about fixing tissues — it’s about restoring trust in movement.
A good rehab plan considers:
Tissue healing and nervous system behavior
Strength and tolerance
Mechanics and confidence
When therapy addresses both the physical and neurological components of pain, outcomes improve.
The Bottom Line
Pain does not always mean harm.
Pain does not always mean something is wrong.
Pain does not mean you’re broken.
Sometimes it means your nervous system is doing its job a little too well.
With the right guidance, education, and gradual progression, that system can calm down — and movement can feel safe again.